According to leading fertility experts in the USA, In Vitro Fertilization (IVF) continues to be one of the most effective solutions for couples facing infertility challenges. IVF is a medical procedure where an egg and sperm are combined outside the body, and the resulting embryo is carefully transferred into the uterus to achieve pregnancy. Over recent years, advancements in reproductive technology have made IVF safer, more accessible, and increasingly successful than ever before.
Dr. Emily Carter, a renowned reproductive endocrinologist based in New York, notes that IVF isn’t just about medical science—it’s about offering hope to millions of couples who dream of becoming parents. She stresses that understanding the process, preparation, and potential outcomes is crucial before starting treatment.
At Home Healthy Remedy, we aim to guide you through every stage of IV F—from the initial consultation and diagnostic tests to embryo transfer and post-procedure care. Whether you are beginning your fertility journey or considering advanced options, this comprehensive guide will help you make informed decisions with confidence.
What Is IVF and How Does It Work?
In Vitro Fertilization (IVF) is an advanced fertility treatment that helps individuals or couples conceive when natural conception isn’t possible or has been unsuccessful. The term “in vitro” means “in the lab,” referring to the process of fertilizing an egg with sperm outside the body. Once fertilization occurs, the healthiest embryo is carefully placed into the woman’s uterus, where it can develop into a pregnancy.
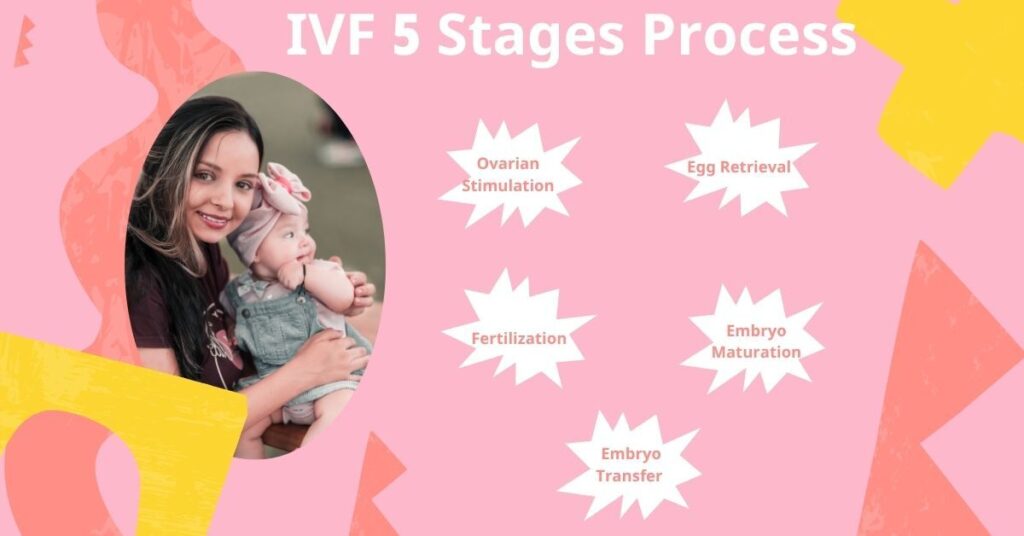
According to fertility specialists, IVF typically involves several key steps:
- Ovarian Stimulation: Hormonal medications are given to help the ovaries produce multiple mature eggs.
- Egg Retrieval: A minor procedure is performed to collect the eggs from the ovaries.
- Fertilization: The eggs are combined with sperm in a controlled lab environment.
- Embryo Culture: The resulting embryos are monitored for several days to identify the strongest ones.
- Embryo Transfer: A selected embryo is gently transferred into the uterus.
If the embryo implants successfully, pregnancy begins. I V F offers hope to those facing challenges such as blocked fallopian tubes, low sperm count, endometriosis, or unexplained infertility, making it one of the most trusted reproductive technologies today.
Who Can Benefit from IVF Treatment?
IVF can be a life-changing option for individuals and couples who face challenges in conceiving naturally. It’s most commonly recommended for those with blocked fallopian tubes, low sperm count, ovulation disorders, endometriosis, or unexplained infertility. However, age plays a crucial role in determining IVF success rates.
Women in their 20s to early 30s generally have the highest success rates, as their eggs are more viable and healthier. Between ages 35 and 40, success rates gradually decline due to reduced egg quality and quantity, but many women in this range still achieve pregnancy with proper medical guidance. For women over 40, IVF can still be effective—especially when using donor eggs, which significantly improve the chances of conception.
Men’s age can also impact results; sperm quality tends to decline after age 45, which may affect embryo health.
In summary, IVF benefits a wide range of people, from younger couples with fertility issues to older individuals pursuing parenthood through assisted reproductive technologies. Consulting a fertility specialist can help determine the best approach based on age, health, and reproductive goals.
Step-by-Step Process of IVF
The IVF process involves several carefully monitored stages designed to increase the chances of a successful pregnancy. According to fertility specialists in the USA, the journey typically begins with an initial consultation and fertility evaluation, where both partners undergo tests to assess hormone levels, egg quality, and sperm health.
Once treatment begins, the process usually includes:
- Ovarian stimulation: Fertility medications are prescribed to encourage the ovaries to produce multiple mature eggs.
- Egg retrieval: A minor surgical procedure is performed under sedation to collect eggs from the ovaries.
- Fertilization: Collected eggs are combined with sperm in a laboratory setting to create embryos.
- Embryo culture: The embryos are monitored for several days to ensure healthy development.
- Embryo transfer: A selected embryo is gently placed into the uterus using a thin catheter.
After the transfer, the patient may take hormone support to help with implantation. A pregnancy test is performed about two weeks later to confirm the results. Each step is customized based on individual health needs, ensuring the best possible outcome for every patient.
How to Prepare for Your IVF Journey
Preparing for IVF involves both physical and emotional readiness. According to fertility specialists, a well-prepared patient can improve the chances of success and reduce stress during treatment. Start by scheduling a thorough consultation with your reproductive endocrinologist, who will review your medical history and recommend any necessary tests. Maintaining a healthy lifestyle is essential—this includes a balanced diet, regular exercise, avoiding smoking or excessive alcohol, and managing stress.
Patients should also understand the IVF process and timeline, including medication schedules and monitoring appointments. Emotional support is equally important; consider counseling or joining support groups to navigate the journey with confidence.
Key preparation steps include:
- Completing required diagnostic tests (hormone levels, ovarian reserve, semen analysis)
- Discussing medication plans and potential side effects
- Planning for time off work and daily routines during treatment
- Ensuring a support system of family or friends
By focusing on both health and knowledge, couples can enter IVF with realistic expectations and a proactive mindset, setting the stage for a smoother and more hopeful journey.
Common Tests Before Starting IVF
Before beginning I V F, fertility specialists recommend a series of essential tests to evaluate both partners’ reproductive health and increase the chances of a successful outcome. For women, common tests include hormone level assessments such as FSH, LH, AMH, and thyroid function tests, which help determine ovarian reserve and overall fertility. A transvaginal ultrasound is often performed to assess the uterus and ovaries, while screening for infections and genetic conditions ensures the safety of the procedure.
For men, a semen analysis is conducted to evaluate sperm count, motility, and morphology. Additional tests, such as hormone profiling or genetic screening, may be recommended if previous fertility issues are detected.
Key tests at a glance:
- Hormone level testing (FSH, LH, AMH, thyroid)
- Transvaginal ultrasound of ovaries and uterus
- Infection and genetic screenings
- Semen analysis for male partners
By completing these tests, doctors can personalize the I V F treatment plan, identify potential challenges early, and improve the likelihood of a successful pregnancy.
Success Rates and Factors That Influence IVF Results
IVF success rates can vary significantly depending on several key factors. On average, women under 35 have the highest chances of success, often ranging from 40% to 50% per cycle, while success rates gradually decline with age. Egg quality, sperm health, and underlying fertility issues play a major role in determining outcomes. Lifestyle factors such as smoking, excessive alcohol use, and obesity can also negatively impact success. Additionally, the clinic’s experience, laboratory quality, and adherence to advanced protocols contribute to higher pregnancy rates. For some patients, using techniques like ICSI (Intracytoplasmic Sperm Injection) or preimplantation genetic testing (PGT) can improve results, especially in cases of recurrent IVF failure. While no treatment guarantees pregnancy, understanding these influencing factors can help couples make informed decisions and set realistic expectations before starting IVF.
Possible Side Effects and Risks of IVF
While IVF is generally safe, fertility specialists emphasize that it can involve certain side effects and risks that patients should be aware of. The most common mild side effects include bloating, cramping, mood swings, and temporary fatigue, usually related to hormonal medications. Some women may experience injection site reactions or mild ovarian tenderness.
More serious but less common risks include:
- Ovarian Hyperstimulation Syndrome (OHSS): A rare condition where the ovaries become swollen and painful due to stimulation medications.
- Multiple Pregnancy: IVF increases the chance of twins or triplets, which can lead to higher pregnancy complications.
- Ectopic Pregnancy: In rare cases, the embryo may implant outside the uterus.
- Procedure-related complications: Though uncommon, egg retrieval or embryo transfer can carry minor surgical risks.
Dr. Emily Carter advises that understanding these risks, maintaining regular communication with your fertility clinic, and following post-procedure care instructions can significantly reduce complications and improve the overall IVF experience.
Emotional and Mental Health During IVF
IVF is not only a physically demanding process but also an emotionally challenging journey for many couples. Fertility treatments often involve uncertainty, hormonal changes, and repeated procedures, which can trigger stress, anxiety, and mood fluctuations. According to Dr. Emily Carter, addressing mental health is just as important as the medical aspect of IVF, as emotional well-being can indirectly influence treatment outcomes.
Some common emotional challenges during IVF include:
- Anxiety and fear about the procedure or results
- Emotional highs and lows due to hormone medications
- Feelings of isolation or pressure in social and family settings
To support mental health, experts recommend:
- Seeking counseling or therapy specialized in fertility issues
- Practicing stress-reduction techniques, such as meditation, yoga, or journaling
- Building a support network with partners, friends, or IVF support groups
By proactively managing emotional health, couples can navigate IVF with greater resilience, clarity, and hope, improving their overall experience during this life-changing journey.
Latest Advancements in IVF Technology (2025 Update)
IVF technology continues to evolve rapidly, offering higher success rates and more personalized treatment options. In 2025, several key advancements are transforming the IVF experience for patients:
- Improved Embryo Screening: Modern genetic testing allows doctors to identify the healthiest embryos, reducing the risk of genetic disorders and increasing implantation success.
- Artificial Intelligence (AI) in Embryo Selection: AI algorithms analyze embryo development patterns, helping embryologists select embryos with the highest chances of success.
- Advanced Cryopreservation Techniques: Vitrification has improved, allowing eggs and embryos to be frozen with higher survival rates for future use.
- Personalized Hormone Protocols: Fertility specialists can now tailor hormone stimulation plans based on a patient’s unique ovarian response, optimizing results.
These innovations not only improve outcomes but also reduce emotional and physical stress during IVF. According to Dr. Emily Carter, embracing these cutting-edge technologies gives patients “the best chance of success while minimizing risks.”

